Background
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is an effective therapy for acute leukemia (AL) with the potential to achieve long-term remission. Nevertheless, relapse remains the main cause of mortality after allo-HSCT. Isolated extramedullary relapse (iEMR) is defined as the presence of clonal blasts in tissues other than the medullary compartment, in the absence of bone marrow relapse (BMR) and with full donor chimerism. Reports on its prevalence and risk factors are rare and its implications on prognosis and treatment continue to be an area of active study. Our aim was to describe the rates, clinical characteristics, and outcomes of patients with iEMR in the post-allo-HSCT setting.
Methods
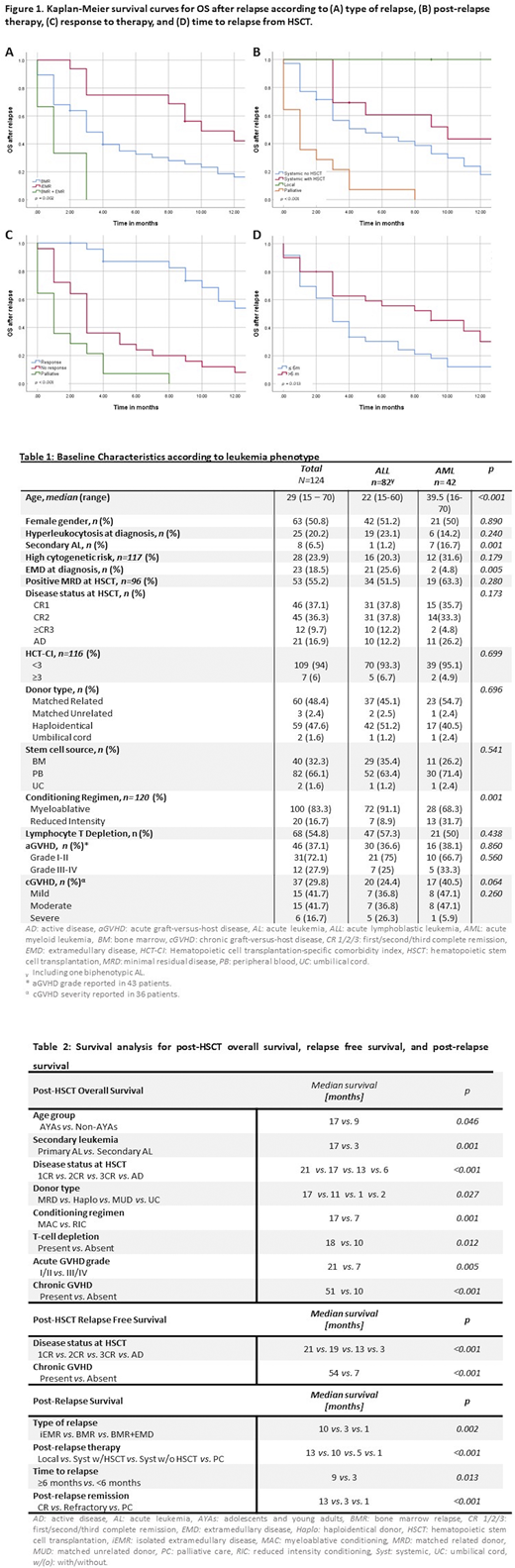
Retrospective multicenter study that included patients ≥15-years-old diagnosed with AL who underwent allo-HSCT with chemotherapy-only conditioning regimens between 1999-2019. Patients referred to participating centers after HSCT and those with incomplete medical records were excluded. The Kaplan-Meier method was used to construct survival curves, differences between groups were analyzed using the log-rank test, and a standard Cox-regression was carried out for multivariate analysis.
Results
One hundred twenty-four patients were included with a median follow-up of 12 months (1-158) after allo-HSCT. The most common AL phenotype was lymphoblastic (ALL) in 66.1% (n=82). High-risk cytogenetics were present in 23.9% (n= 28). Twenty-three patients (18.5%) had a history of extramedullary disease (EMD) prior to allo-HSCT, CNS being the most common site in 52.2% (n=12). Additional baseline characteristics are presented in Table 1.
Median overall survival (OS) for the cohort was 15 months (1-158). Factors related to decreased OS on univariate analysis are shown in Table 2. Independent risk factors for mortality were: belonging to the non-AYA group (HR 4.7,95%CI 1.6-13.3; p=0.004), grade III-IV acute GVHD (HR 3.9, 95%CI 1.6-9.8; p=0.003), and absence of chronic GHVD (HR 10.3, 95%CI 3.4-30.9; p<0.001).
Sixty-seven patients (54%) relapsed after allo-HSCT with a median time to relapse of 13 months (1-158). Of these, 19 (28.4%) had EM involvement, of which 16 (23.9%) had iEMR. All cases of iEMR occurred in patients with ALL. The most commonly involved EM sites were CNS in 47.3% (n=9), skin in 26.3% (n=5), and breast in 15.8% (n=3). Of patients with post-allo-HSCT CNS relapse, 85.7% (n=6) had prior history of pre-HSCT CNS EMD. Post-relapse therapy was administered to 76.1% (n=51), including a second allo-HSCT in 25.5% (n=13), the remaining patients transitioned to palliative care.
Median relapse free survival (RFS) was 13 months (1-124). Factors demonstrating a protective role are described in Table 2. On multivariate analysis, early disease stage at time of HSCT (HR 0.35, 95% CI 0.18-0.71; p=0.003) and the development of chronic GVHD (HR 0.29, 95% CI 0.15-0.54; p<0.001) had a positive impact on RFS.
The median OS after relapse was 4 months (2.6-5.3). Factors related to increased survival on univariate analysis are described in Table 2 and in Figure 1. On multivariate analysis, an iEMR (HR 0.13, 95% CI 0.026-0.67; p= 0.015), as compared to a relapse with a medullary component, and a complete remission after post-relapse therapy (HR 0.095, 95%CI 0.039-0.233; p<0.001) positively impacted OS.
Conclusion
Isolated EMR was highly prevalent in our population as compared to historical cohorts. This reflects differences in Latin American AL epidemiologic distribution, with high representation of ALL, and our limited access to conditioning regimens based on total body irradiation. Patients that had an iEMR and achieved treatment response had improved survival outcomes which may reflect a more indolent biology allowing the clinician time to implement therapy intensification interventions. Additionally, in our setting, escalation of pre-HSTC therapy to achieve deeper responses and tailoring HSCT, in combination with post-HSCT CNS prophylaxis, are potential strategies that should be pursued further.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal